Monoamniotic twins (monochorionic and dichorionic): what to fear for the expectant mother. Monoamniotic twins (monochorionic and dichorionic): what to fear for the expectant mother Monochorionic diamniotic twins
Diamniotic dichorionic twins are not uncommon these days. Statistics show that most often such multiple pregnancies occur in women aged 35 to 39 years. The reasons for such fertilization are considered to be hormonal disorders in the body, including hormonal stimulation in the process of treating female diseases. Such twins are born in 30% of multiple pregnancies. If the incidence of twins is correlated with the number of singleton pregnancies, then for every 100 normal births there are 4-5 diamniotic dichorionic twins.
What are diamniotic dichorionic twins?
In medicine, there are four types of twins, which occur only with two methods of conception:
- When two eggs are fertilized by two different sperm at the same time or with an interval of up to a week. Each baby is in a separate amniotic sac and has its own placenta. This pregnancy is called diamniotic dichorionic twins. Children can have different genders and different appearances.
- When the egg is divided into two full parts after a certain period of time after fertilization. If division occurred within 2-3 days, each fetus may have a separate amniotic sac and its own placenta. If the division occurred at a later period, the babies will have both the chorion and amnion in common. Only the chorion or only the amniotic sac may be common. This pregnancy is called monoamniotic). Children have the same set of chromosomes and the same appearance and gender.
Dichorionic diamniotic twins by week

It is possible to determine the presence of twins using hardware only from the 5-6th week of pregnancy. A gynecologist can suspect the presence of two babies during an examination only from the 9-10th week. Only at this time the uterus begins to grow more intensively and does not match its size in time. Pregnancy with twins is most often accompanied by early toxicosis. It is much more severe than in a singleton pregnancy and may return at a later stage. This type of pregnancy is more optimal for mother and children than monochorionic pregnancy. Let's look at how diamniotic dichorionic twins develop week by week.
First trimester
- 1-4 weeks do not differ from a singleton pregnancy, the only thing is that toxicosis can appear a week after fertilization.
- 5-8 weeks: Each baby is about 2 cm long by the end of the 8th week. Taurus are fully formed. Fingers have appeared, but they still have membranes. The umbilical cord has formed, the placenta is still developing. Mom has toxicosis. This is the most dangerous period for miscarriage.
- 9-12 weeks: time The examination will confirm that the woman has diamniotic dichorionic twins. Babies begin to develop teeth, and by the end of their term, their genitals are formed. The babies are already 6 cm long each and weigh 6-9 g. By the end of the 12th week, the likelihood of miscarriage decreases.
Second trimester

- 13-16 weeks: a pregnant woman’s belly visually looks 2 two weeks longer than during a singleton pregnancy, it is already clearly visible. The babies move actively, frown, suck fingers, sleep a lot, and wake up about once an hour.
- 17-20 weeks: babies push well with their legs and arms, they are about 25 cm tall and weigh 300 g. Children’s intestines are already fully functioning, they independently pee in the amniotic fluid, which is renewed several times a day. Polyhydramnios may occur.
- 21-24 weeks: The lungs begin to mature. A pregnant woman may experience back pain and swelling in her legs. Children weigh 600 g. During this period, an ultrasound is performed, the sex can be determined, the presence or absence of congenital defects can be diagnosed; dichorionic diamniotic twins are clearly visible in the photo.
Third trimester
- 25-28 weeks: children accumulate fat, the nervous system, vision and hearing are formed. In the mother, the fundus of the uterus rises 30 cm from the pubis.
- 29-32 weeks: babies are about 37 cm tall and weigh 1.3-1.6 kg. During this period, an ultrasound is performed, which allows you to determine the readiness of babies for birth, detect abnormalities in the chorion and omnion, predict and plan the course of labor.
- 33-36 weeks: babies weigh about 2 kg, their heartbeat is about 120 beats per minute. The head of one child drops down, the second is most often in a breech position. By the 36th week, a woman can give birth at any time.
- 37-40 weeks: babies are completely ready to be born; in height and weight they lag behind their singleton peers. Most often, babies will appear at 37-38 weeks. There is a high probability of planned continuation of pregnancy before childbirth. By this period, the mother’s weight increases by 15-17 kg.
Can a woman do it on her own?

If a woman has dichorionic diamniotic twins, childbirth can occur either naturally or with assistance. Everything depends on the course of pregnancy and associated complications. If a pregnant woman has a severe form of late toxicosis, gestosis, severe varicose veins and other aggravating troubles, there is a high probability of a cesarean section. Caesarean section is performed for transverse or both babies. The decision is made by doctors based on repeated ultrasound results and observations of the course of pregnancy. The optimal condition for natural childbirth is cephalic presentation of both babies; cephalic presentation of one of them and foot presentation of the other is also acceptable. In other cases, there is a high probability of performing a cesarean section.
Twins and ultrasound

If dichorionic diamniotic twins are suspected, an ultrasound photo confirms this fact only from 5-6 weeks. At later stages (32-36 weeks), you can technically “lose” one child. This happens because one baby overlaps the second one during an ultrasound and the latter becomes invisible to the device. Pregnancy with twins requires more frequent ultrasound examinations due to the risk of developing pathologies and complications in babies. The examination allows you to establish:
- type of zygosity of twins;
- vitality of children;
- future labor management tactics;
- pronounced pathologies of children or one of them;
- the presence of polyhydramnios or oligohydramnios in each of them;
- biometric parameters, degree of development, compliance with gestational age;
- the death of one of the fetuses at any stage allows you to save the second child under favorable conditions; the probability of developing pathology and defects in a living baby is no more than 10%.
Dangers of twins

Dichorionic diamniotic twins develop more favorably than monozygotic twins. This is due to the fact that babies have separate amniotic sacs and placentas; they do not depend on each other. However, such children also face dangers. One of them is the freezing of one of the fruits. There is no need to worry about this. If the death occurs during or later, the dead fetus becomes mummified, which is not dangerous for the woman in labor and the second child. The second danger is the likelihood of polyhydramnios due to the fact that through the shunt between the placentas, blood is discharged more strongly to one of the babies, which is why the baby pees more often, and polyhydramnios gradually develops. In this regard, children may vary in weight. Starting from the 32nd week, babies begin to lag behind in height and weight. This is not dangerous for children; this fact does not affect mental and physical development in any way. The lag is due to the fact that there is little space left in the uterus. After birth, babies will quickly catch up with the weight and height of their peers.
Hi all! I’m writing this mostly for myself, while everything is fresh in my memory) this pregnancy was not planned for us, of course this does not mean that it was not wanted. I found out that we were expecting twins at the first ultrasound at 5 weeks. There we saw 2 fertilized eggs, of course the hearts were not beating yet, but the embryos were already beginning to be poorly visualized. And then my quiet life came to an end, I was worried about absolutely everything. For 2 days I cried from a state of shock, I could not even imagine that this could happen to me. A week later, at an ultrasound, we were told that both of our hearts were beating, and with twins and even a scar on the uterus after the first cesarean, it was time to register, which I couldn’t do right away, 2 clinics didn’t want to take responsibility, so they fed me breakfast, In the end, they gave me a referral to the residential complex at the PC. And I became registered at 10 weeks. Overall, the pregnancy was going well. All tests are always good, ultrasound too, the babies developed according to their due date, the difference between them was a week, but for twins this is normal. At 12 weeks I was told that we were expecting boys) until week 20 I had terrible toxicosis, I felt sick all the time and usually in the evenings. After the 20th week and until the end, I couldn’t eat normally because I had nowhere to go, food was a lump in my throat. At 20 weeks it was already difficult for me to walk. At 33 weeks I had the flu, I needed to drink, and I treated the flu with oscillococcinum (((from about that time I began to fall apart. At 34-35 weeks the bones separated to such an extent that it seemed they were not connected to each other in any way and were all were mobile, it was hard to breathe, eat, lie down, whatever, everything was hard. And I felt terrible, I hadn’t slept at night for a long time, I couldn’t walk normally, I walked along the wall and dreamed of a walker or a wheelchair. I gained 16 kg. And at 36 weeks and 6 days we went for a planned hospitalization at the maternity home, we were supposed to go at 37 weeks, but it was already scary to stay at home. My husband was already leading me there, I could barely walk. The examination made me happy, informing me that I was already in labor and my 3rd finger was dilated. I went through the standard procedures, lay under a CTG. Then they took me to the operating room. The operation lasted no more than an hour, but this hour seemed like an eternity. I felt lousy, I was either sick or afraid, and my anesthesiologist decided to knock me out after the babies were delivered. During the operation, it turned out that my uterine scar from the first ECS had already begun to disperse and I arrived on time. Ignat was first born at 13:36 with a weight of 2600 and 48cm 7/8 Apgar. Second Matthew 13:38 with a weight of 2600 and 48cm 8/9 Apgar. Exactly the same in weight and height, but so different in appearance) they don’t look a bit alike, Ignat is dark-haired, long-haired, he looks very much like me, and Matvey is white, has short hair and looks like his dad) They told me about the children, showed them and I fell asleep here. They woke me up at the end of the operation. Already in the intensive care unit they told me that the first of the twins was transferred to the neonatal intensive care unit because the child was moaning. In the evening they brought Matvey to me to feed. I was able to get up after midnight; I couldn’t let go of one leg for a long time. Of course, I’m a sissy and I feel sorry for myself, when they understood me, I screamed to be put in my place))) And the next day I was transferred to the postpartum room with Matveyka. I went to the intensive care unit to see Ignat, and there they told me that the child had an intrauterine infection, suspected pneumonia and hypoxia. He was lying in an incubator, they gave him oxygen, my poor little blood, and all because I had the flu and didn’t know how to be treated correctly (((all on IVs, there are those pens, there’s no wreath, and they put wreaths in my head and temple, a terrible sight, my heart was breaking. Coming from the intensive care unit, I cried, cried and prayed, the doctors didn’t really tell me anything, every day he was consistently heavy and that’s all. They fed him through a tube, because he was spitting up a lot and we ruled out Pneumonia. They treated only infection and hypoxia. I suffered from horror when I approached the usual place where my son’s incubator stood, before I had time to open it, the nurse shouted to me that my child was not there, saying that you don’t see that the incubator is large and connected to the devices (mine? Ignatushka was not connected to the devices) and then the ground disappeared from under his feet. What happened to him? It turned out that they simply moved him to another place. And when on the 6th day I came to my son and saw that he had neither a probe nor a probe. One dropper made me cry out loud, now I know what real tears of happiness are! The most important thing is health! Our health and that of our babies! For 7 days we lay separately from each other, Matveyka with me and Ignatushka in intensive care, and then we were transferred to the neonatal pathology department. Of course, Ignat was thinner, his cheeks were sunken, you couldn’t look at them without tears, there were also abrasions on his cheeks from the plaster with which they glued the probe, and the tyrants tore it off along with the skin (((In pathology, we were prescribed peracetam and a full examination, x-ray, ultrasound of the hearts, head, abdominal cavity, ECG, blood and urine tests. The jaundice was illuminated under lamps and discharged home after 10 days. The eldest son was at home with his grandmothers and dad all this time. Everyone reassured me, saying that mothers usually endure separation more difficult than children, but that was not the case. By the time I was discharged, Zakharka became so sad that his temperature asymptomatically rose to 39 and lasted for several days and 2 days after my discharge, he screamed in his sleep for 1.5 months, very loudly and loudly, called me and did not respond when I approached him, it didn’t stop the hysteria. He still asks me to feed him, even with what he can eat himself, he is afraid of losing sight of me. Now everything has stabilized and seems to be back to normal. I can’t tell you how many tears were shed for the children, both the twins and the older one! I just started talking about this more calmly, before I started talking about Zakharka’s condition, I cried and couldn’t help myself. The twins are soon 2 months old) we’ll just go to the clinic, we were told to get stronger a little at home) our grandmothers and husband are helping with the kids) for now we are on guard duty occasionally, when we don’t get enough, I can supplement with a little formula, but I hope that soon lactation will improve and we will have enough) mothers who breastfed twins, tell us how long you fed them?) maybe there are some secrets that you can do to get more milk?) we are still walking in our arms, since we had a problem choosing a stroller (see last post) girls! Take care of yourself and your children! Treat yourself correctly! Good health to everyone! After all, this is the most important thing!
Diamniotic twins- this is the simultaneous presence in the uterus of two fetuses, each of which has its own amniotic sac. Despite the increase in the number of multiple pregnancies, diamniotic twins are still rare: on average, only one in eighty pregnancies is a multiple.
As you know, the basis of future life is the egg. It matures in the ovary, and then leaves it and rushes to the fallopian tube. If on its way through the tubal cavity it meets a sperm, the fusion of two cells occurs - fertilization. As a result, a multicellular structure is formed - a zygote. Intensively fragmenting, the zygote descends through the tube into the uterine cavity and penetrates the endometrium for further development. More often, fertilization occurs with the participation of a single egg and one sperm, so in the end a single embryo appears, and the pregnancy ends with the birth of one child.
Two embryos may appear in the uterus if:
— Two eggs are involved in fertilization. As a rule, it happens alternately in one or the other ovary, so usually one ovary manages to “grow” a single full-fledged egg in one menstrual cycle. Another situation is also possible, when two mature follicles are formed in one ovary at once, which become the source of two full-fledged eggs. Once they enter the fallopian tube, they can be fertilized instantly.
Sometimes, over a period equal to one menstrual cycle, ovulation occurs symmetrically in both ovaries, that is, when one of the ovaries “does not rest.” In this scenario, two eggs each end up in their own fallopian tube, and fertilization occurs symmetrically on both sides.
The simultaneous presence of two mature eggs is not a pathology, but is rarely observed.
The result of symmetrical fertilization of two eggs at once is the appearance of two independent zygotes/embryos, which is why twins are called dizygotic or fraternal. Born children have a different gene set and a different phenotype, that is, they can be different sexes and different from each other, therefore they are called twins.
— A single egg is fertilized, but then at the zygote stage it is divided in two in such a way that a full-fledged embryo is formed from each half. Since both halves of the zygote are completely identical in their set of genes, the children born (monozygotic, identical) are always of the same sex and similar in appearance, that is, they are twins.
Statistically, fraternal (dizygotic) children are born more often.
How do two embryos subsequently develop in the uterus? The pregnancy development scenario is initially determined by the number of fertilized eggs. If each embryo had its own “own” egg, then the fetus will subsequently have an individual placenta with membranes and a separate amniotic sac (amnion). More often (70%) this is how a twin pregnancy develops.
A different situation is observed in cases where the source of the development of two embryos is a single egg, which is split into two. Both embryos begin to develop thanks to a common placenta, but their amniotic sac can be either common or separate for each.
If the egg divides early (on days 3–8), each embryo receives an individual amniotic membrane and, accordingly, its own amniotic sac. Late division always results in two embryos in one amniotic sac.
The course and outcome of a twin pregnancy is determined by its type. The most favorable option is considered to be that each fetus has its own placenta and its own amniotic sac.
What are diamniotic twins?
The most likely circumstances that provoke a twin pregnancy are known. These are:
— Genetically determined predisposition to the simultaneous birth of two children. The presence of twins in a family does not necessarily mean the birth of twins in all relatives, but it significantly increases this probability.
- Age. The largest number of twin pregnancies is registered in women who have overcome the 30-year mark. It is assumed that such statistics can be explained by the natural decline of hormonal ovarian function. A decrease in the number of ovulations provokes the deposition of hormones, which act as hyperstimulants during the ovulatory cycle.
— Long-term use of hormonal drugs for the purpose of contraception. The contraceptive effect of these drugs is based on the suppression of ovulation. According to the withdrawal symptom, after stopping oral contraceptives, the ovaries begin to intensively stimulate ovulation.
— Artificial, extracorporeal, conception. Afterwards, twin pregnancies are not uncommon, since the procedure itself involves the introduction of several fertilized eggs into the uterine cavity so that the most viable of them ultimately survives. Sometimes, as a result, two (less often more) embryos begin to develop.
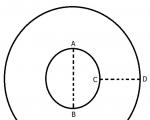
The development of diamniotic twins means that each fetus has its own amniotic sac. Such twins may have one placenta (chorion), then the twins are considered monochorionic, and if each of the children has their own place for children, the twins are considered dichorionic.
Any development of diamniotic twins is characterized by two isolated amniotic sacs. When they come into contact, they form an interfertal septum.
The option with a single placenta and a single amniotic sac (monochorionic monoamniotic twins) is rare. With this type of pregnancy, both fetuses develop in a single amniotic sac in the absence of an interfetal septum, so often both fetuses end up fused.
The development of dichorionic diamniotic twins can be observed in an abnormally formed uterus. With some malformations, the uterus turns out to be doubled, and the vagina and cervix can double with it. If only the body of the uterus is doubled, the organ acquires. When both uterine halves are fully functioning, they can carry a pregnancy symmetrically, and each of the developing embryos will eventually receive its own placenta and isolated amniotic sac.
Monochorionic diamniotic twins
If the division of the egg begins 3-8 days after its fertilization, then each of the two formed embryos ultimately has an isolated amnion, but the placenta remains the only one for both.
In the case of a normal, singleton pregnancy, the fetus is surrounded by two membranes - chorionic and amniotic. The chorionic membrane, in the form of a dense membrane, surrounds the outside of the fetal receptacle and is tightly attached to the fetal part of the placenta. The amniotic lining is essentially the wall of the amniotic sac. The placenta and membranes are called the placenta because they leave the uterus after the fetus.
In the case of monochorionic diamniotic twins, each embryo is surrounded by its own amniotic membrane, but has a common placenta, so the interfetal septum is formed in two layers, and a single chorionic membrane covers them only from the outside.
The placenta is a unique structure, temporarily created by nature to provide all the vital functions of the developing fetus. Thanks to the placenta, namely its ability to secrete progesterone, it is not interrupted prematurely. It also supplies the fetus with oxygen, elements of immune defense, vitamins, and minerals. All harmful waste products of intrauterine life of the fetus are also eliminated by the placenta. The source of everything necessary for the fetus is the mother’s body, and the intermediary is the placenta. In the area where the baby's place is attached to the uterine wall (placental area), the placenta penetrates deeply into the endometrium with the help of peculiar villi (chorionic villi), forming depressions for the exchange of maternal and placental blood. At this point, the placenta receives the necessary substances and transports them to the baby through the umbilical cord - a long, rope-like formation that connects the placenta and the fetus. The umbilical cord includes vessels and excretory canals, it is attached to the central part of the placenta, and its other end grows into the anterior abdominal wall (umbilical area) of the child. Regardless of the variant of twin pregnancy, each of the fetuses present in the uterine cavity always has an individual umbilical cord.
The placenta has the characteristic of “aging”. Since the lifespan of the placenta is limited by the period of gestation, by the time of birth its resources are completely depleted. It is logical to assume that if it is necessary to ensure the intrauterine development of two fetuses at once, it is extremely difficult for a single placenta, and its resources are depleted prematurely. Therefore, against the background of monochorionic diamniotic pregnancy, hypoxia (oxygen starvation) and developmental delay are often diagnosed in fetuses.
A high load on the chorion during monochorionic pregnancy can contribute to premature pregnancy.
A twin pregnancy is a serious test for the woman herself, regardless of the location of the fetuses.
Dichorionic diamniotic twins
The development of dichorionic diamniotic twins begins in the first three days after fertilization of a single egg. Two embryos are formed, two amions and two chorions/placentas, and the septum between the fetuses has four layers. This option of twins is most favorable for children, since each of them has an isolated development zone and its own placenta. However, the burden on the mother's body remains very high.
The course of a twin pregnancy differs from that with one fetus in the uterus. Since two fetuses require from the mother’s body twice as much of all the substances and oxygen necessary for development, the volume of circulating blood (CBV) must increase enough to meet this need. If during a singleton pregnancy the blood volume increases by 40%, then during a twin pregnancy this figure approaches 60%, and this is accompanied by an increased load on the vascular system. Carrying twins is often accompanied by severe edematous syndrome and.
During any pregnancy, BCC is replenished solely by increasing the volume of plasma, which does not contain iron reserves and, accordingly, hemoglobin. We can say that a pregnant woman’s blood is “diluted” due to the liquid part, as a result, the hemoglobin level drops, which is why it occurs. As a rule, in a singleton pregnancy, if it develops properly, minor anemia is considered physiological, because the pregnant woman’s body can cope with it. The presence of two fetuses increases the amount of circulating blood even more, so severe anemia is diagnosed in almost all pregnant women with twins.
The presence of two placentas (hyperplacentosis) during dichorionic pregnancy provokes early and late toxicosis in almost half of patients with twins. Toxicoses form very early and are more pronounced.
A uterus that is too large with twins inside increases the load on adjacent organs that are under pressure.
In a singleton pregnancy, the signal for the onset of labor is the enlargement of the uterus to a certain size and the downward displacement of the fetus. With twins, the uterus becomes large earlier than the “proper” period, so labor often starts already at the 37th week.
When carrying twins, their asymmetrical development is possible, when one of the embryos develops with a lag. The development of dichorionic diamniotic twins is most favorable in this regard, since each embryo has its own amniotic sac and chorion.
Birth of monochorionic diamniotic twins
Even in the case of the most successful course of a twin pregnancy, regardless of the nature of the location of the fetuses, it requires a special attitude from a specialist, both during development and during childbirth.
Naturally, every patient pregnant with twins is interested in the question of the method of childbirth. The opinion that diamniotic pregnancy is an indication for surgical delivery is absolutely incorrect. Moreover, often the final decision is made after the patient’s preliminary hospitalization, which is indicated for everyone in case of twins.
Early hospitalization is necessary, first of all, for the expectant mother herself. Carrying twins is accompanied by a significant burden on the woman; on the eve of childbirth, the adaptive resources of her body are depleted, while she has to go through another important and difficult stage -. Prenatal therapy helps the mother's body compensate and rest.
Preliminary hospitalization of a patient with a diamniotic pregnancy is also necessary for obstetricians. In order to have a reliable picture of the development of pregnancy and assess all upcoming risks, diagnostic measures are carried out to assess the possibility and safety of independent childbirth, and if this is not possible, to plan the date and method of the operation. During the examination, the following are assessed:
— What type of twin pregnancy is this? Ultrasound scanning allows you to see the number of placentas and amnions.
- Location of fruits. In order for the fetus, as in the case of singleton births, to safely pass the birth canal, it must be positioned vertically, preferably head down (cephalic presentation); an oblique and transverse position does not imply a natural birth. In case of twins, both fetuses should leave the uterus in a vertical position. It is desirable that both move their heads down, however, if the second fetus has the buttocks presented, the birth also proceeds normally: after the birth of the first, the second fetus is “rotated” under ultrasound control to the required position.
— Fruit sizes. The uterine muscles are not able to push out two large fetuses at once, especially in fragile pregnant women.
— The degree of development and readiness for “ectopic” life of both fetuses. There are situations when twins develop asymmetrically, and one of the children is underdeveloped (hypotrophy) or even non-viable.
As already mentioned, it is often diagnosed during twin pregnancies. If it is severe, natural childbirth can worsen oxygen deprivation and lead to serious consequences.
Childbirth with monochorionic diamniotic twins has a main feature - both fetuses communicate with a single placenta, which often fails to cope with the task. More often, with this type of development, fetuses show signs of hypoxia and malnutrition, so natural childbirth is too severe a test for them. Also, monochorionic twins may be accompanied by:
- Reverse arterial perfusion syndrome, when twins have only one heart. As a result, a fetus with only one heart has a vascular and.
— Fetofetal transfusion syndrome. Subject to physiological development, each fetus is connected to the placenta by individual vessels. If there is a disturbance in the development of the vessels of one of the fetuses, it “joins” the vessels of the other fetus through anastomoses. As a result, the blood of one fetus is dumped into another, so the “donor” has developmental abnormalities.
Thus, children with a single placenta are often less hardy, and the risks of spontaneous childbirth during monochorionic pregnancy are almost always high. Therefore, such pregnancies often end with a cesarean section.
No matter how frightening the listed complications may seem, it should be clarified that they are rare.
Birth of dichorionic diamniotic twins
Dichorionic diamniotic twins are essentially double a “normal” pregnancy, with each baby having its own fluid (amniotic fluid) and placenta. It is this type of pregnancy that often ends in natural childbirth, especially if the pregnancy proceeded with minimal complications.
If both fetuses are symmetrically developed and healthy, the birth of dichorionic diamniotic twins proceeds similarly to that of a singleton pregnancy, only in the end two children and two placenta are born. However, even the most successful twin pregnancy often ends earlier, so pre-hospitalization is also recommended for dichorionic twins.
In what situations is it recommended to give birth to dichorionic diamniotic twins operatively?
— Incorrect position of one/both fetuses. The pelvic location of the first of the children and the transverse position of the next will not allow them to be born.
— Presence of large fruits. As a rule, a special diet is recommended for those carrying twins so that, while they have all the necessary nutrients, the children do not gain excess weight.
— Uncompensated complex gestosis: stable arterial hypertension, severe proteinuria.
— Signs of increasing hypoxia of one or both fetuses.
— Signs of placental abruption in any of the children.
— Lack of proper psychological readiness of the pregnant woman herself for the upcoming difficult birth.
A positive psychological attitude of a woman in labor before childbirth, with any number of fetuses in the uterus, is extremely important, since all labor activity is controlled by the central nervous system. Fear of pain and possible complications can provoke disruption of the normal birth process. Unfortunately, often pregnant women with twins themselves insist on surgical delivery, and if the doctor fails to convince them, such a wish is granted.
Multiple pregnancy always pleases and frightens parents at the same time. But it is unlikely that any of them, at the moment of announcing such a diagnosis, think about the fact that a couple in the womb can develop completely differently.
In obstetrics and gynecology, several types of twins are distinguished, and the rarest of them is monoamniotic twins, which are formed already in the first days (from the 7th to the 13th) after fertilization. How will these babies be born and what to expect from childbirth? It is better for parents to find out all the information about this in advance.

First, parents need to find out what it is - monoamniotic twins, in order to have a correct understanding of the intrauterine development of babies. The fact is that with such a multiple pregnancy, they have one amniotic sac (amniotic fluid) between them. Accordingly, they will divide among themselves:
- substances to protect the immune system that are produced by the amniotic sac;
- amniotic fluid;
- space.
Accordingly, the closest possible connection is established between the kids. They come into contact with each other, feed on the same substances. One might assume that they will be almost the same in everything, but in reality this is not always the case. Sometimes this is fraught with complications during childbirth, which it is also advisable for parents to know about in advance. Even monoamniotic twins are classified in medicine.
Famous twins. Among the star couples are actresses Olga and Tatyana Arntgolts, football players Vasily and Alexey Berezutsky, actors James and Oliver Phelps (the red-haired brothers from Harry Potter), models Mary-Kate and Ashley Olsen, tennis players Bob and Mike Bryan, and the well-known “Electronics” - Vladimir and Yuri Torsuev.
Species

It is incorrect to believe that the amniotic sac and the placenta are one and the same. The first is the fetal membrane, which contains the baby during pregnancy. It is filled with a biologically active liquid medium. The placenta is an embryonic organ that communicates between the fetus and the mother. Monoamniotic twins have one amniotic sac between them, but the placentas may be different. Depending on this intrauterine factor, the following types of twins are distinguished:
- monochorionic monoamniotic twins - children develop in the same amniotic fluid and are nourished from the same placenta;
- monoamniotic dichorionic twins - despite the fact that the babies are in the same membrane, they have different placentas (the prefix di- or bi- means “two”).
The fact that both fetuses develop in the same amniotic sac already poses a danger for them, since there may not always be enough nutrients for two. And if twins also have only one placenta, this complicates the entire process of intrauterine development even more. So in this regard, more favorable prognoses await dichorionic monoamniotic twins. How are such children born?
Wow! Even the encephalograms of monoamniotic twins are as similar as possible. That is, their brains work the same way.

Naturally, the question arises of what such children will look like. Doctors define their description and degree of similarity unambiguously: both mono- and dichorionic monoamniotic twins will have the same:
- chromosome set;
- blood type;
- appearance.
As a rule, even parents find it difficult to distinguish such children by their appearance. It is these twins who often even have the same location of moles, and they get sick at the same time. And the spiritual, internal connection in monoamniotic twins is, as a rule, very close. So much so that they feel each other at a distance, even if they live in different places. They fall in love at the same time and die with a small gap in time. However, before the happy moment of their birth, parents will have to experience many difficulties. This is not only the rarest type of twins, but also the most dangerous.
This is interesting! Even the DNA of monoamniotic twins is as similar as possible. However, there is a feature that will be completely different between them. These are fingerprints.
Complications

You should not count on an easy birth with monoamniotic twins. You need to set yourself up from the very beginning, as soon as you heard this diagnosis, that the babies will appear through. To avoid dangerous moments during delivery, doctors in such cases always resort to surgical intervention. And here it is 100% justified. How scary the forecasts sound, but it is among monoamniotic twins that the mortality rate exceeds 50%.
What complications are fraught with this multiple pregnancy?
- Entwined with umbilical cords
Since monoamniotic twins develop in one amniotic sac, and the length of their umbilical cords is traditional (about 50 cm), the most common complication is. Moreover, each of the children can get confused both in their own and in someone else’s. The result is hypoxia and even death. One person or two may die at once.
- Interweaving of umbilical cords
Both babies are actively moving inside the same amniotic sac. If they do not accidentally wrap themselves in umbilical cords, then there is a great danger that their umbilical cords will become intertwined. The result is that nutrients can no longer be supplied to small organisms, and the children will die.
- Lack of nutrition
It is difficult for one mother’s body, which should normally feed one child during pregnancy, to bear two. The nutrients contained in the amniotic fluid may not be enough for one of the twins. The result of this is pathology in the development of one of the fetuses and even death due to lack of adequate nutrition.
- Underdevelopment
The most common complication when carrying monoamniotic twins is the death of one of the children due to the fact that the second, due to its greater vitality and activity, absorbs more nutrients than its brother (or sister). Accordingly, it develops faster in the mother’s womb, grows and gains weight. While the second one in his shadow remains weak. This can lead to his death or prematurity.
- Siamese twins
If the twins are not only monoamniotic, but also monochorionic, it is quite possible that the twins are fused by some part of the body. The survival rate of babies in such cases is minimal, but it is quite possible for them to be born safely. Today, surgeons have successful experience in separating conjoined twins, after which they live full lives, separately from each other.
According to statistics, monoamniotic twins are born only in 1 case out of 100 twins. The chances of survival for both babies are slim, but they exist. Modern medicine has experience in handling even such complex births. The mechanism of such conception has not yet been fully studied; the reasons for this phenomenon can only be assumed, but they have no scientific justification.
Interesting fact. Most often, twins are born to women of the Negroid race. Whereas in Asia such cases are extremely rare.
About the reasons
The same statistics claim that monoamniotic twins are born most often in the following cases:
- mother's age after 35 years;
- the mother has been taking contraceptive hormonal drugs for too long;
- genetics (if multiple pregnancies are a pattern in the family);
- having many children;
- deviations in the structure of the uterus.
Monoamniotic twins are diagnosed already at the first ultrasound. A competent specialist rarely makes a mistake in making such a diagnosis. Parents should not be afraid if this is their case. With regular visits to the gynecologist and following all his recommendations, you can bear and give birth to full-fledged and healthy children. And then be proud that they are so individual, unlike everyone else, but completely identical to each other.