Modern problems of science and education. Pirogov Waldeyer's lymphadenoid pharyngeal ring Lymphoid ring
Lymphoid ring (Pirogov–Waldeyer ring)– a complex of 6 pharyngeal tonsils.
Tonsilla lingualis(lingual)– a set of lymphoid follicles of the posterior part of the tongue.
Tonsilla palatina(palatines)– steam room, located in fossa tonsillaris, formed by arcus palatoglossus, and arcus palatopharyngeus. Surrounded by a fibrous capsule.
Tonsilla pharyngea(palatal/adenoids) - an accumulation of lymphoid tissue at the border between the upper and posterior walls of the pharynx, along the midline.
Tonsilla tubaria(pharyngeal)- a paired accumulation of lymphoid tissue between the pharyngeal opening of the tube and the soft palate.
That. at the entrance to the pharynx there is an almost complete ring of lymphoid formations: tonsil of the tongue, 2 palatines, 2 tubes and pharyngeal.
This organ requires a more detailed description. In addition to 4 tonsils, there are accumulations of adenoid tissue in the form of diffuse and limited formations scattered throughout the pharyngeal mucosa. These include the so-called grains of the posterior wall of the pharynx, the lateral ridges of the pharynx and similar formations in the area of the nasopharyngeal openings of the Eustachian tubes.
Palatine tonsils They represent great diversity in their shape and size. The outer surface of the palatine tonsil, covered with a thin connective tissue capsule, is adjacent directly to the wall of the pharynx, in a special bed. The inner surface of the tonsil, facing the lumen of the pharynx, is pitted with crypts or lacunae of various depths and shapes. The lower pole of the tonsil hangs freely over the root of the tongue.
Upper pole almost closely approaches the angle formed by both arches, leaving space for a triangular depression - fossa supratonsillaris. This supramindal fossa, according to the observations of Orleans, sometimes represents a deep cavity located in the thickness of the soft palate (recessus palatinus) and containing an additional lobe of the tonsil. In some cases, in the thickness of the soft palate there is a tree-like branching canal - sinus tourtual, which essentially represents the deep crypt of the tonsil. These anatomical options are of great importance in clinical practice.
Blood supply to the tonsils deserves special attention. The tonsil artery has a different origin, as can be seen in the attached Bulatnikov diagram.
Lymph circulation of the tonsils. The tonsils represent a peripheral lymphadenoid apparatus, similar to Peyer's patches and solitary intestinal follicles. The tonsils do not have afferent lymphatic pathways. There is no lymph flow from inside the tonsils to its surface. On the contrary, the phenomena of absorption from its pharyngeal surface are observed in the amygdala. The lymph flow from the tonsil goes centripetally and is directed to the corresponding regional lymph nodes.
pharyngeal tonsil, located along, is cut by deep grooves, which extend quite symmetrically on both sides of the median groove. Thus, the entire amygdala is divided into separate lobules. In the posterior part of the median sulcus there is a small depression called the bursa pharyngca.
4th amygdala, located between the root of the tongue and the epiglottis, it represents an accumulation of lymphoid tissue of varying sizes. In pathology it plays the least role. parapharyngeal space, made of loose fiber, it is divided by a special connective tissue plate, together with the muscles attached to the styloid process, into 2 sections. In the anterior section there are: art. maxillar. int., n. auriculo-temporalis, n. lingualis and n. alveolaris inferior, and in the thickness of the parotid gland - the external carotid artery. In the posterior section: internal carotid artery, jugular vein, 9th, 10th, 11th and 12th cephalic nerves and lateral trunk of the sympathetic nerve.
Features of the structure of the palatine tonsils: The functional organization of the palatine tonsils is closest to that of Peyer's patches; in them there is direct close contact of lymphoid elements with the epithelium. The tonsils take part in the implementation of “local” (in the oropharynx) nonspecific immune reactions,
The lymphoepithelial ring of the tonsils represents the body's first line of defense against the introduction of pathogenic microorganisms. This is where the delay and neutralization of dangerous agents occurs. It is an important component of the human lymphatic and immune systems.
The structure of the pharyngeal ring
These are accumulations of lymphatic tissue, which is penetrated by connective tissue stroma. The lymphoid pharyngeal ring consists of 6 tonsils:
- Paired palatine and tubal.
- Single pharyngeal and lingual.
The palatine tonsils are located on the sides of the basal part of the tongue in the depths of the oropharynx. Normally, they are not visible during normal visual inspection. Only if the palatine tonsils are inflamed and enlarged will we be able to see them by sticking out our tongue.
Tubal tonsils are located deep in the ridges that surround the openings of the auditory (Eustachian) tubes. These pipes connect the cavity of the inner ear and the pharynx, which makes it possible to equalize the pressure (during holtania).
Localization of the pharyngeal tonsil is the place of transition of the posterior wall of the pharynx to the upper one. In children, it has a predisposition to hyperplasia (overgrowth). This makes nasal breathing difficult and the child has a constant open-mouthed facial expression and snoring. This condition is called adenoids.
The lingual tonsil is located in the thickness of the mucous membrane covering the root of the tongue.
When examining the tissues of the ring under a microscope, you can notice accumulations of immune cells - lymphocytes. In the center of the nodules that they form there is a reproduction zone, closer to the periphery there are more mature cells.
The mucous membrane of the tonsils is covered with stratified epithelium, which is not prone to keratinization. It forms numerous invaginations (crypts) deep into the tonsil parenchyma. This creates additional area for contact with pathogenic material.
In humans, these formations reach their peak development at 5–6 years. At this time, mucous immunoglobulins, which have antibacterial and antiviral properties, begin to be actively secreted.
When a child reaches adolescence, the intensity of tonsil functioning decreases. This occurs due to the acquisition of an active form of immunity to many diseases. There is a process of reverse development of the tonsils, which is a physiological norm.
Immune function
When microbes enter our upper respiratory tract, the first barrier for them is the mucous membrane, on the surface of which there is secretory IgA, and in its thickness there are immune cells. The tonsils become the center of reproduction of these cells. Thus, the Pirogov ring provides local immune reactions for the nasopharynx and oropharynx.
The processes of ensuring cellular and humoral immunity take place here. T-lymphocytes participate in cellular reactions. They detect cells with “foreign” receptors and phagocytose (absorb) them. However, such a system is not effective for all microorganisms. A more complex mechanism - humoral - involves the participation of B lymphocytes and the production of specific antibodies against the pathogenic agent.
Until 3–4 years of age, T cells predominate in the parenchyma of the components of the Pirogov-Waldeyer lymphoepithelial ring, and at school age, B cells predominate.
Due to such disturbances in the ratio of lymphocyte populations, their ability to secrete immunoglobulins is impaired. This, in turn, leads to frequent incidence of infectious diseases and the tendency of the tonsils to inflammation and hyperplasia - enlargement.
The immune response pattern is as follows:
- Capture of a pathogenic microorganism by reticular epithelial cells.
- Its absorption by antigen-presenting cells (they break up the antigen into particles and display them on their surface). This makes it possible to “familiarize” other immune cells with information about the “enemy”.
- Antigen-dependent proliferation and differentiation of B lymphocytes.
- Transformation of some B-lymphocytes into plasmacytes - cells that synthesize antibodies against the presented antigen.
- Another part of the B lymphocytes turns into memory B lymphocytes. They contain information about the antigen and circulate in the blood for a long time (years), providing a secondary immune response when the antigen re-enters the body.
Cells of the mononuclear phagocytic system – macrophages – take part in the process of inactivation of dangerous microorganisms. They absorb foreign particles and dead cells. Macrophages also synthesize components of the nonspecific immune system: interferon, blood complement, hydrolytic enzymes, etc.
An important component of complex immune defense is mucus, which covers the mucous membranes of the nose, mouth and pharynx.
It contains polysaccharides that can block receptors on the surface of microorganisms. When this happens, they lose their ability to adhere (if the microbe does not adhere to the epithelium, then its pathogenicity will not be realized). Mucus and saliva also contain lysozyme, an enzyme that breaks down the cell wall of bacteria, making them vulnerable.
Other features

In the tissues of the lymphoid ring of the pharynx, the function of hematopoiesis, namely lymphopoiesis, is also realized. The tonsils have a dense network of capillaries, as well as excretory lymphatic ducts that connect them to the general lymphatic system. Once formed, differentiated lymphocytes (those that carry information about the antigen) migrate to nearby lymph nodes, and then to the bloodstream and the central organs of the lymphatic system - the thymus and spleen.
Lymphocytes are capable of exiting into the lumen of the pharynx to the surface of the mucous membrane, where they can provide protection to the body.
The Pirogov ring is closely connected with other body systems. This connection is realized through the plexuses of the autonomic nervous system. For example, with prolonged tonsillitis (inflammation of the tonsils) there is a risk of developing heart failure. In addition, the purulent process in the crypts of the tonsils is a source of infection. Tonsils that cannot cope with their functions are recommended to be removed surgically or subjected to cryodestruction - a treatment method using liquid nitrogen.
The relationship between the lymphoepithelial ring and the endocrine system has been proven. With excessively active production of adrenal hormones (glucocorticoids, mineralocorticoids), hypertrophy of the tonsils is observed. And vice versa, when the level of these hormones in the blood decreases, the tonsils atrophy - they become smaller. This connection is inverse: during a sore throat, the synthesis of glucocorticoids (stress hormones) is stimulated, which help mobilize the body's defenses.
Classification of tonsillitis by I. B. Soldatov
Classification of chronic tonsillitis by B. S. Preobrazhensky
Classification of chronic tonsillitis by L. A. Lukovsky
Complications of sinusitis
Local purulent-inflammatory processes:
- Rhinogenic intraorbital complications
- Intracranial
- Osteomyelitis of the frontal bone or upper jaw.
Intraorbital complications: contact route of penetration – the presence of common thin bone walls with the orbit. Hematogenous route (via the anterior and posterior ethmoid artery and vein).
Clinical picture:
- General symptoms: general inflammatory, intoxicating
- Rhinogenic symptoms (nasal boil, abscess of the nasal septum, signs of purulent sinusitis).
- Orbital features:
Reactive edema - often in children with pathology of the soft tissues of the nose, sinusitis, emoiditis, etc. An initial, non-purulent process. Painless, mild swelling.
Osteoperiostitis of the orbital wall - pain in the orbital area increases with pressure on the orbital globe, with movement of the eyeballs, scleral injection, etc.
Subperiosteal abscess - everything that is characteristic of osteoperiostitis in combination with displacement of the eyeballs upward (if the maxillary sinus), downward (if frontal sinusitis), laterally - with ethmoiditis. An abscess bulging into the orbital cavity.
Retrobulbar abscess - severe pain, severe exophthalmos, limited mobility of the eyeballs.
Phlegmon of the orbit - exophthalmos, ophthalmoplegia (complete immobility), etc.
Treatment: surgical opening of the causative sinus through external access, surgical intervention on the tissues of the orbit. With appropriate therapeutic treatment (very intensive).
Suggests distinguishing three forms of chronic tonsillitis:
A. Compensated.(This form represents a dormant site of chronic infection of the tonsils.)
B. Subcompensated.(frequent exacerbations are observed. Due to a significant decrease in the general reactivity of the body and its allergization, there is a state of unstable, incomplete compensation.
B. Decompensated.(Decompensated chronic tonsillitis includes forms that occur with local and general complications (parotonsillitis, parapharyngitis, tonsillogenic intoxication), and forms of chronic tonsillitis that occur with tonsillogenic infectious-allergic diseases of organs and systems (rheumatism, nephritis).
I. Simple form. This includes cases of chronic tonsillitis that occur only with local symptoms, subjective complaints and objective signs of the disease, with frequent sore throats, and in other cases - without repeated sore throats (“non-angina” chronic tonsillitis).
II. Toxicallergic form. Occurs as a result of a violation of protective and adaptive mechanisms. This includes forms of chronic tonsillitis that occur with low-grade fever and symptoms of tonsillogenic intoxication; Tonsillo-cardiac syndrome, etc. is often diagnosed. The importance of toxic-allergic manifestations varies, and therefore it is advisable to distinguish between grade 1 (with milder symptoms) and degree 2 (with significantly more pronounced phenomena).
I. Acute.
1. Primary: catarrhal, lacunar, follicular, ulcerative membranous tonsillitis.
2. Secondary:
a) for acute infectious diseases - diphtheria, scarlet fever, tularemia, typhoid fever;
b) for diseases of the blood system - infectious mononucleosis, agranulocytosis, alimentary-toxic aleukemia, leukemia.
II. Chronic.
1. Non-specific:
a) compensated form;
b) decompensated form.
2. Specific: for infectious granulomas - tuberculosis, syphilis, scleroma.
Pathoanatomical classification of chronic tonsillitis V. N. Zak
1. Chronic superficial tonsillar lacunit, ulcerative or non-ulcerative. The inflammatory process is localized mainly in the lacunae of the tonsils.
2 A. Chronic parenchymal tonsillitis (acute). The greatest changes are observed in the lymphadenoid tissue (foci of softening, blurring of the boundaries of the follicles).
2 B. Superficial chronic parenchymal sclerotic tonsillitis. The abundant proliferation of connective tissue in the parenchyma of the tonsils comes to the fore.
3. Deep chronic parenchymal sclerotic tonsillitis.
The lymphoepithelial pharyngeal ring is a large accumulation of lymphoid tissue in the mucous membrane of the upper respiratory tract, which includes the pharyngeal, lingual, laryngeal, tubal and palatine tonsils, as well as single follicles scattered in the mucous membrane of the oropharynx and pharynx. There are accumulations of lymphoid tissue on the posterior and lateral walls of the pharynx, in the pyriform sinuses and in the area of the ventricles of the larynx.
The lymphoid apparatus in the pharynx is located in a ring-like manner, which is why it was called the “lymphadenoid pharyngeal ring” by Waldeyer-Pirogov.
Signs, distinguishing palatine tonsils from other lymphoid formations of the pharynx:
· In the palatines in the tonsils there are lacunae that turn into crypts, which branch in a tree-like manner up to 4-5 orders and spread over the entire thickness of the tonsil, while in lingual and pharyngeal In the tonsils there are not crypts, but grooves or clefts without branches.
· Lymphoepithelial symbiosis has its own characteristics: in all tonsils, except the palatine tonsils, it extends only to their surface. In the palatine tonsils, the lymphoid mass is in contact with the epithelium on a large surface of the crypt walls. The epithelium here is easily permeable to lymphocytes and antigen in the opposite direction, which stimulates the production of antibodies.
· The palatine tonsils are surrounded by a capsule - a dense connective tissue membrane covering the tonsil on the lateral side. The lower pole and pharyngeal surface of the tonsil are free from the capsule. The pharyngeal and lingual tonsils do not have a capsule.
· In the paratonsillar tissue of the upper pole of the palatine tonsils, Weber's mucous glands are sometimes located, which do not communicate with the crypts.
· Lymphadenoid tissue undergoes reverse development over time. The pharyngeal tonsil undergoes involution starting from 14-15 years of age, the lingual tonsil reaches its maximum development by 20-30 years. Involution of the palatine tonsils also begins at 14-15 years of age and persists until old age.
The main function of the tonsils is is the formation of lymphocytes - lymphopoiesis. Lymphopoiesis occurs in the centers of the follicles, then, upon maturation, lymphocytes are pushed to the periphery of the follicles, from where they enter the lymphatic pathways and the general lymph flow, as well as onto the surface of the tonsils. In addition to follicles, the formation of lymphocytes can also occur in the lymphoid tissue surrounding the follicles.
They also take part in formation of immunity(antibody formation), especially at a young age. This is facilitated by the fact that the location of the palatine tonsils on the path of the main entrance gate for various infectious pathogens and toxic products ensures close contact of the mucous membrane of the tonsils with the bacterial agent, and this, in turn, underlies the formation of immunity. The very structure of the crypts - their narrowness and tortuosity, the large total surface of their walls - contributes to long-term contact of antigens and lymphoreticular tissue of the tonsil.
Palatine tonsils perform elimination function by participating in the removal of excess lymphocytes. The large area of contact between lymphadenoid tissue and the epithelium in the crypts plays an important role in the migration of lymphocytes across the surface of the mucous membrane of the tonsils, maintaining a constant level of lymphocytes in the blood.
Many researchers admit enzymatic function tonsils of the pharyngeal ring, in particular the palatine tonsils. Biochemical analyzes made it possible to detect various enzymes in the tissue of the tonsils, as well as in migrating lymphocytes - amylase, lipase, phosphatase, etc., the content of which increases after eating. This fact confirms the participation of the palatine tonsils in oral digestion.
TONSILS (tonsillae) - accumulation of lymphoid tissue in the thickness of the mucous membrane at the border of the nasal, oral cavities and pharynx. Depending on the location, there are palatal M. (tonsillae palatinae), pharyngeal M. (tonsilla pharyngea), lingual M. (tonsilla lingualis), and tubal M. (tonsillae tubariae). They form the main part of the Pirogov-Waldeyer pharyngeal lymphoepithelial ring (Fig. 1). In addition to M., this ring includes accumulations of lymphadenoid tissue embedded in the mucous membrane of the outer parts of the posterior wall of the oropharynx, parallel to the velopharyngeal arches, the so-called. lateral ridges of the pharynx, as well as single follicles scattered in the mucous membrane of the pharynx (folliculi lymphatici pharyngei). M. are part of a single lymphoepithelial apparatus that develops in the mucous membrane of the digestive, respiratory, and genitourinary systems in the form of solitary lymphatic follicles (folliculi lymphatici solitarii) or group lymphatic follicles (folliculi lymphatici aggregati). During the process of phylogenesis, the accumulation of lymphoid tissue in the mucous membrane at the border of the pharynx and the oral and nasal cavities in the form of M. was first noted in mammals.
Embryology
M.'s anlage occurs during the prenatal period of development in the area of the head intestine. There is a certain sequence in their formation and development. First of all, the palatine, then the pharyngeal, lingual and tubal M. appears. The palatine M. are laid at the bottom of the second gill pouch at the end of the 2nd - beginning of the 3rd month in the form of a protrusion of the endoderm. The latter gives rise to the epithelial cover and crypt system of the M. Lymphoid tissue of the M develops from the surrounding mesenchyme. At the 8th month of intrauterine development of the fetus, lymphatic follicles of the M. (folliculi lymphatici tonsillares) appear, and by the end of the 1st month of the child’s life, they appear reproduction centers (centrum multiplicationis). Pharyngeal M. is formed in the 3rd-4th month in the form of 4-6 folds of the mucous membrane in the area of the pharyngeal vault. At the 6th month, lymph follicles appear for the first time, and at the 2nd - 3rd month after birth, reproductive centers appear. Lingual M. is formed as a paired formation in the 5th month in the form of longitudinal folds of the mucous membrane of the root of the tongue. At the 6th month, the folds fragment, at the 7th month, follicles appear, and at the 3rd - 4th month after birth, reproductive centers appear. Tubal M. are formed in the 8th month in the form of separate accumulations of lymphocytes around the pharyngeal opening of the auditory tube. By the birth of a child, follicles are formed, and in the first year of life, reproductive centers are formed.
Anatomy
Palatal M. is a paired formation located in the M. pits (fossae tonsillares) of the lateral walls of the pharynx between the palatoglossus arch (areus palatoglossus) and the velopharyngeal arch (areus palatopharyngeus). It has an oval shape, its long axis runs from top to bottom and somewhat from front to back. In a newborn, the size of the palatine m. in the vertical direction is 10 mm, in the transverse direction 9 mm, thickness 2.1 mm; in an adult, respectively, 15-30 mm, 15-20 mm, 12-20 mm. In the palatal M., two surfaces are distinguished: internal (free) and external, facing the wall of the pharynx. The inner surface is uneven, covered with a mucous membrane, has 8-20 irregularly shaped tonsillar dimples (fossulae tonsillares), which are the mouths of tonsillar crypts (cryptae tonsillares), which, branching, penetrate the thickness of the palatine membrane. The crypts increase the free surface area of each palatine membrane up to 300 cm2. When swallowing, the palatine membranes are slightly displaced, and their crypts are freed from their contents. The outer surface of the palatine membranes is covered with a capsule (capsula tonsillae) up to 1 mm thick; on it lies a layer of loose paratonsillar tissue, the edges go down to the root of the tongue, in front it communicates with the tissue of the palatoglossal arch, at the top - with the submucous base of the soft palate. In an adult, the distance to the internal carotid artery from the upper pole of the palatine M. is 28 mm, from the lower pole 11-17 mm, to the external carotid artery 41 mm and 23-39 mm, respectively. The upper corner of the M.'s fossa remains free and is called the supratonsillaris fossa. Sometimes there is an additional palatine M. - the palatine lobe of the palatine M., the edges can extend deep into the soft palate and not have a direct connection with the main palatine M. (Fig. 2). In these cases, it represents an additional intrapalatine M. (tonsilla intrapalatina accessoria), the edges usually contain a deep branched crypt - the sinus of Tourtuali, which plays a certain role in the pathology of the M.
Pharyngeal M. (syn.: nasopharyngeal M., Lushka's tonsil, third M.) is located on the border of the upper and posterior walls of the pharynx (see), has the appearance of a round-shaped plate with 4-8 folds of the mucous membrane diverging on its surface, protruding into the cavity nasopharynx. The pharyngeal M. is well developed only in childhood; with the onset of puberty, its reverse development occurs.
lingual M. (syn. fourth M.) is located in the region of the root of the tongue (see), occupying almost the entire surface of the root of the tongue. Its shape is often ovoid, the surface is uneven, and lingual follicles (folliculi linguales) are located on the mucous membrane, divided by grooves into a number of folds. M.'s crypts are shallow, at the bottom of many crypts the excretory ducts of the salivary glands open, the secretion of which helps to wash and cleanse the crypts. In a newborn, the lingual M. is well developed, its size is longitudinal 6 mm, transverse 9 mm. After 40 years, a gradual reduction of lingual M occurs.
Pipe M. is a paired formation, which is an accumulation of lymphoid tissue in the thickness of the mucous membrane of the nasopharynx at the pharyngeal opening of the Eustachian tube (see Auditory tube). In a newborn, the tubal M. is well defined, approx. 7.5 mm, diameter approx. 3.5 mm. Tubal M. reaches its greatest development at 5-7 years of age; later it gradually atrophies and becomes almost invisible.
The blood supply of the M. lymphoepithelial pharyngeal ring, including the palatine M. (Fig. 3), is carried out by arterial branches (aa. tonsillares), extending directly from the external carotid artery or its branches: the ascending pharyngeal (a. pharyngea ascendens), lingual (a. . lingualis), facial (a. facialis), descending palatine (a. palatina descendens). M.'s veins are formed in the parenchyma, accompany the arteries and flow into the pharyngeal venous plexus (plexus venosus pharyngeus), lingual vein (v. lingualis), and pterygoid venous plexus (plexus venosus pterygoideus). M. does not have afferent lymphatic vessels. The draining lymph vessels flow into the lymph nodes: parotid, retropharyngeal, lingual, submandibular. M.'s innervation is carried out by the branches of the V, IX, X pairs of cranial nerves and the cervical part of the sympathetic trunk. In the subepithelial layer of connective tissue septa, M.'s parenchyma, there are individual nerve cells, their clusters, pulpy and non-pulpate nerve fibers, various types of nerve endings, and extensive receptor fields. The blood supply and innervation of the muscle change with age.
Histology

M. consist of stroma and parenchyma (Fig. 4). The stroma forms the connective tissue framework of M., formed by collagen and elastic fibers. They form a capsule (shell) around the M.’s circumference, from which connective tissue crossbars (trabeculae) extend into the M.’s depth. In the thickness of the crossbars there are blood and lymphatic vessels and nerves of the M., and sometimes the secretory sections of small salivary glands. M.'s parenchyma is represented by lymphoid tissue (see), the cellular basis of the cut is lymphocytes, macrophages, and plasma cells. Elements of lymphoid tissue form in some places round-shaped clusters - follicles, which are located parallel to the epithelium along the free surface of the tumor and along the crypts. The centers of the follicles can be light - the so-called. reproduction centers, or reactive centers. The free surface of the M. is covered with a mucous membrane with multi-row squamous non-keratinized epithelium. In the area of the crypts it is thinner and in places broken; the basement membrane is also fragmented, which contributes to better contact of the lymphoid tissue with the environment.
Physiology
Having a common structure with other lymphatic organs (see Lymphoid tissue), M. perform similar functions - hematopoietic (lymphocytopoiesis) and protective (barrier). The follicular apparatus, embedded in the mucous membranes, is a lymphoid barrier, biol, whose role is the neutralization of toxic substances and inf. agents that enter mucous membranes from the environment. In human M. there are both thymus-dependent and thymus-independent populations of lymphocytes (see), which carry out reactions of both cellular and humoral immunity (see). M. are a peripheral organ of immunity that has a certain uniqueness. Firstly, they have a lymphoepithelial structure, secondly, they are the entrance gates for microbial antigens and, thirdly, they lack lymphatic vessels. It is known that M. contain cells that produce antibodies of the IgE class, which are believed to perform a protective function. It has been shown that lymphocytes of M.'s lymphoid tissue produce interferon (see), which is a nonspecific factor of antiviral immunity.
Research methods
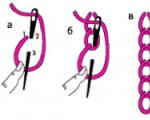
M. can be examined with posterior rhinoscopy (see) - pharyngeal and tubal, with pharyngoscopy (see) - palatine, lingual, lateral ridges and lymphoid follicles (granules) of the posterior wall of the pharynx. The method of palpation and probing of lacunae is used. The palatal m. are examined by rotating or dislocating them using two spatulas, and the contents of the lacunae and its nature are determined. There is usually no content in the M. lacunae of a healthy person. The M.'s rotation is performed with a tonsillorotator or a wire spatula, which is pressed on the palatoglossus (anterior palatine) arch, which entails the rotation of the M. with the free surface forward. In this case, the mouths of the lacunae open and their contents are squeezed out - plugs, pus (Fig. 5).
Pathology
Developmental anomalies. Developmental anomalies include the palatine lobule and the accessory palatine M. Sometimes, instead of one palatine M, two M develop on each side. Additional lobules hanging on the stem have been described. As a rule, these anomalies do not require treatment.
Damage- burns, wounds of M. are rare in isolation; more often they are combined with internal and external injuries of the pharynx (see).
Foreign bodies- most often fish bones, which can penetrate into the muscle tissue, causing pain when swallowing. Remove them with tweezers or special forceps. After removal, a disinfectant rinse and a gentle diet are recommended for one to two days (see Foreign bodies, pharynx).
Diseases
Acute disease of palatine M. - spicy tonsillitis , or sore throat(cm.). Chron, inflammation of the palatine M. - tonsillitis (see). Hyperplasia of the palatine membranes occurs in children; there are no signs of inflammation. M. are only increased in size. If hyperplasia causes difficulty breathing or swallowing, children undergo surgery - tonsillotomy (Fig. 6), i.e. partial cutting off of the protruding part of the M. Before the operation, a full wedge examination is necessary.
The operation is low-painful, most often done without anesthesia, on an outpatient basis, with a special instrument - a guillotine knife - a tonsillotome, the size of which is selected according to the size of the removed muscle. Hyperplasia of the palatine muscles is in most cases accompanied by the proliferation of adenoid tissue of the nasopharynx, therefore tonsillotomy is often combined with adenotomy (see . Adenoids). Bleeding after tonsillotomy is usually minor and stops quickly. The child should remain under medical supervision for 2-3 hours. It is recommended to observe bed rest for 1-2 days, then semi-bed rest for 3-4 days. Food should be liquid and mushy, at room temperature.
Acute inflammation of the pharyngeal M., or acute adenoiditis(see), observed mainly in children. In this case, the tubal M. may also be involved in the inflammatory process. Inflammation is catarrhal, follicular or fibrinous in nature. Due to the anatomical proximity of the mouth of the auditory tube, symptoms of tubo-otitis may occur (see).
Isolated disease of the lingual M. is much less common. It occurs in middle-aged and elderly people and may be accompanied by an abscess of the lingual M.; occurs with high fever, difficulty swallowing and speaking, and severe pain when protruding the tongue.
With angina of the lateral ridges of the pharynx, inflammation occurs in the lymphoid follicles scattered along the back wall and in the lateral lymphoid ridges (columns). Often a whitish dotted coating appears on individual follicles of the posterior pharyngeal wall.
A disease of the lymphoid tissue of the larynx is called laryngeal sore throat; it is manifested by high fever, general malaise, sharp pain when swallowing food and palpating the larynx area. Plaques are often visible, and there may be swelling of the outer ring of the larynx (see Laryngitis).
In addition to the primary lesion of M., changes in the lymphoid tissue of the pharyngeal ring occur in blood diseases. With leukemia (see), infectious mononucleosis (see Infectious mononucleosis), lymphogranulomatosis (see), an increase in palatal M. can cause difficulty breathing and swallowing. Ulcerative changes in the palatine muscles, such as necrotizing tonsillitis, are also possible.
With syphilis, the palatine M. are affected in all stages of the disease. There are descriptions of hard chancroid M.: against a limited hyperemic background in the upper part of M. a hard infiltrate appears with painless erosion in the center, the edges soon turn into an ulcer with compacted edges and bottom; the lesion is unilateral, characterized by regional lymphadenitis (see). In stage II of syphilis, syphilitic tonsillitis occurs: round or oval plaques, separate and confluent, appear on the muscle, rising above the surface of the muscle, surrounded by a reddish rim, easily ulcerating; characterized by bilateral lesions; the entire M. is enlarged, dense, covered with plaque; Papules are found on the mucous membrane in the corners of the mouth, on the palatine arches, and along the edge of the tongue. In stage III, gumma can lead to the disintegration of M., which threatens bleeding from large vessels. Treatment - see Syphilis.
Primary M. tuberculosis is rare; its main symptom is difficulty swallowing and nasal breathing as a result of concomitant M. hyperplasia. Secondary M. damage can be observed in patients with pulmonary tuberculosis. Both forms can occur hidden, simulating a banal chronic condition, tonsillitis. Treatment - see Tuberculosis.
Tumors
There are benign and malignant tumors of M. Benign tumors can be epithelial - papilloma (see Papilloma, papillomatosis), adenoma (see) and non-epithelial connective tissue - fibroma (see Fibroma, fibromatosis), angioma (see), lipoma (see. ); neurogenic - neurinoma (see), chemodectoma (see Paraganglioma), myogenic - fibroids (see). Malignant tumors can also be epithelial - squamous cell carcinoma, glandular carcinoma, undifferentiated transitional cell carcinoma (see Cancer), lymphoepithelioma (see) and non-epithelial - sarcoma (see), fibrosarcoma (see). angiosarcoma (see), chondrosarcoma (see), reticulosarcoma (see) and lymphosarcoma (see).
Most palatal tumors are characterized by slow growth, moderate hyperemia, and mild induration over a long period of time. Squamous cell carcinoma is characterized by ulcerative-infiltrative growth. Sarcoma is characterized by a slowly progressive increase in M. with ulceration in the late period. The transitional cell form of cancer and lymphoepithelioma are characterized by rapid growth with the involvement of surrounding tissues, early regional and distant metastasis. The initial symptoms of the tumor are difficulty swallowing, the sensation of a foreign body in the throat, and an increase in muscle mass; later pain occurs when swallowing, radiating to the ear, lower jaw, and neck. Tumors of the palatine M. can spread to the soft palate, arches, lateral wall of the pharynx, and root of the tongue.
When pharyngeal M. is affected, patients complain of difficulty breathing through the nose, ear congestion, and hypersecretion of mucus with ichor appears. When the tumor disintegrates, bleeding and an unpleasant odor occur. The tumor quickly metastasizes and grows into the cranial cavity. Biopsy results are decisive in diagnosis. Benign tumors of M. are treated surgically. For malignant tumors, due to their high radiosensitivity and tendency to early metastasis, radiation therapy is indicated.
Radiation therapy for malignant tumors of M. is carried out by the method of external radiation therapy using gamma installations, linear electron accelerators, and betatrons. Additionally, intraoral close-focus radiotherapy is used (see Radiation therapy).
In the absence of metastases, in addition to the tumor and the area of its most likely subclinical spread, the area of the retropharyngeal, submandibular, upper and middle deep cervical lymph nodes is also irradiated. In case of metastases on the affected side or on both sides of the neck, all lymph nodes up to the level of the clavicle are irradiated, respectively, on one or both sides.
Irradiation of the primary focus is carried out using a static (2-4 fields) or rotational mode, and lymph nodes of the lower parts of the neck - from one or two anterior or anterior and posterior fields. The larynx, trachea and spinal cord are protected with lead blocks. The total doses to the primary tumor focus and metastases are 5000-7000 rad (50-70 Gy) for 5-7 weeks, while it is advisable to deliver 1000-1200 rad (10 - 12 Gy) directly to the tumor area from the target fields, and to zones of subclinical tumor spread 4000-4500 rad (40-45 Gy) in 4-4.5 weeks. Radiation therapy begins only after sanitation of the oral cavity (see). During irradiation, substances that mechanically, thermally and chemically irritate the mucous membrane are excluded from the diet.
Simultaneously with radiation, chemotherapy is carried out with cyclophosphamide, olivomycin, 5-fluorouracil, methotrexate, and vinblastine. For highly radiosensitive tumors (eg, lymphoepithelioma, lymphosarcoma), cyclophosphamide, or olivomycin (30-40 minutes before irradiation), or vinblastine (5-10 mg intravenously once every 5-7 days) is used. For relatively radioresistant tumors (for example, squamous cell carcinoma, angiosarcomas, etc.), 5-fluorouracil (30-40 minutes before irradiation) or methotrexate 5 mg daily is used. In cases of relapse or lack of effect, either surgical treatment or repeated courses of chemotherapy are recommended.
During surgical treatment of palatine tumors that do not infiltrate the medial pterygoid muscle, a transoral approach to the tumor is possible. For more common tumors and relapses after radiation therapy, various types of lateral pharyngotomies are performed (see). The widest access, which makes it possible to perform radical surgery, provides a transmandibular approach to the tumor.
Bibliography: Andryushin. Yu. N. On the issue of the afferent lymphatic vessels of the human palatine tonsils, Vestn, otorhinolar., No. 6, p. 74, 1971; Antsy-ferova-Skvirskaya A. A. Conservative treatment of uncomplicated forms of chronic tonsillitis with the use of antibiotics and its objective assessment, Journal, ear., no. and throats, Bol., No. 6, p. 12, 1962; Astrakhan D. B. Radiation treatment of malignant tumors of the oral cavity and oropharynx. M., 1962, bibliogr.; B a z a r n o v a M. A. Cytochemistry of nucleic acids in chronic lymphocytic leukemia, Filatov’s disease and infectious lymphocytosis, Klin, med., v. 44, no. 1, p. 108, 1966; Bondarenko M. N. The role of adenoviruses in the etiology of chronic tonsillitis and acute paratonsillitis in children, Proceedings of the 1st All-Russian. Congress of Otolaryngol., p. 262, M., 1963; Vasilyev A.I. Immunological aspects of the physiology of the palatine tonsils, Zhurn, ushn., no. and throats, Bol., No. 2, p. 10, 1971; Kozlova A. V. Radiation therapy of malignant tumors, M., 1971; Kozlova A.V., Kali-n a V.O. and G a m b u r g Yu. L. Tumors of ENT organs, M., 1979, bibliogr.; Korovina A. M. About the morphogenesis and histochemistry of the palatine tonsils, Vestn, otorhinol., No. 3, p. 105, 1967; Krivokhat-ska Ya L. D. and Povolotsky Ya. L. The role of tonsils in antiviral immunity, in the book: Children's infections, ed. T, G. Filosofova et al., c. 6, p. 98, Kyiv, 1976; K at r and l and N I. A. and Gorbachevsky V. I. About the pathology of the lymphopharyngeal ring in children, Zhurn, ear., no. and throats, Bol., No. 4, p. 57, 1976; Likhachev A. G. The significance of the pathology of the lymphadenoid pharyngeal ring in the etiology, pathogenesis and prevention of other diseases, Proceedings of the 1st All-Russian. Congress of Otolaryngol., p. 140, M., 1963; L about p about t -ko I. A. and Lakotkina O. Yu. Acute and chronic tonsillitis, their complications and connection with other diseases, L., 1963, bibliogr.; Matveeva T. N., Muravskaya G. V. and Melba r d t I. I. Selection of conditions for remote gamma therapy for malignant tumors of the palatine tonsils, Med. radiol., t. 13, no. 11, p. 12, 1968, bibliogr.; M e l l-N"I to P. A. Connections of lymphatic capillaries and lymphatic vessels of the Waldeyer-Pirogov pharyngeal ring, Arch. Anat., Gistol, and Embryol., t. 57, No. 11, p. 83, 1969; Multivolume manual on otorhinolaryngology, edited by A. G. Likhachev, vol. human tonsils, Arch. anat., gistol, and embryol., v. 67, No. 8, p. 39, 1974; Orleansky K. A. Surgical anatomy of the tonsils, Arch. I. et al. Cryosurgery in otorhinolaryngology, M., 1975; Preobrazhensky B. S. and Popova G. N. Angina, chronic tonsillitis
and diseases associated with it, M., 1970, bibliogr.; Guide to microbiological diagnosis of infectious diseases, ed. K. I. Matveeva, p. 298, 350, M., 1973; S i m o l i n V. A. et al. Morphological manifestations of immunological processes in the lymphoid pharyngeal ring in children with respiratory diseases, Vestn, otorhinol., No. 2, p. 55, 1973; Soldatov I.B. About the nervous apparatus of the palatine tonsils, in the same place, No. 6, p. 47, 1953; U n d r Pi c B.F. The importance of the upper respiratory tract in the pathogenesis of allergic diseases, Journal, ear., no. and throats, Bol., No. 4, p. 3, 1960; Falileev G.V. Tumors of the neck, M., 1978; Khechinashvili S.N. and J o r-dania T.S. Study of the patterns of emigration of formed elements of white blood from the palatine tonsils and the pharyngeal mucosa in experiment and clinic, Proceedings of the 5th Congress of Otorhinolaryngology. USSR, p. 475, L., 1959; F i o g e t t i A. Die Gau-menmandel, Darstellung der Biologie und Physiologie, Stuttgart, 1961; Flemming W. Schlussbernerkungen iiber die Zellvermehrung in den lymphoiden Driisen, Arch. mikr. Anat., Bd 24, S. 355, 1885; Mac Comb W. S. a. F 1 e t with h e r G. H. Cancer of the head and neck, Baltimore, 1967; N a u m a n n H. H. Fluoreszenz-mikroskopische Untersuchungen zur Frage der Tonsillenfunktion, Z. Laryng. Rhinol., Bd 33, S. 359, 1954; Parkinson R. H. Tonsil and allied problems, N. Y., 1951; Preobrazhenskii N. A. Angina und chronische Tonsillitis, Stuttgart, 1974; W a 1 d e u e r W. G. tfber den lympha-tischen Apparat des Pharynx, Dtsch. med. Wschr., S. 313, 1884.
N. A. Preobrazhensky; L. F. Gavrilov (an.), G. V. Muravskaya (medical rad.).
Lymphadenoid (lymphatic, lymphoid) tissue is represented by three structural types: a mass of mature lymphocytes, among which relatively rarely there are follicles, which are spherical (oval) in shape with clear boundaries of accumulation of lymphocytes of varying degrees of maturity and reticular connective tissue in the form of a cellular system of trabeculae that supports the mass lymphocytes.
The lymphatic structures of the body are divided into three groups:
lymphatic tissue of the spleen and bone marrow, located in the path of the general blood flow; it is classified as a lymph-blood barrier;
lymph nodes lying in the path of lymph flow; they are classified as a lymphointerstitial barrier. The lymph nodes produce antibodies during infection;
tonsils, along with lymphoid granules of the pharynx and larynx, Peyer's patches and solitary intestinal follicles, belong to the lymphoepithelial barrier, where lymphocytopoiesis and antibody formation occur, and there is close contact between the internal and external environment of the body.
The lymphoid apparatus in the pharynx is located in a ring-like manner, which is why it was called the “lymphadenoid pharyngeal ring” by Waldeyer-Pirogov. It is formed by two palatine tonsils, one pharyngeal or nasopharyngeal, one lingual and two tubal.
There are accumulations of lymphoid tissue on the posterior and lateral walls of the pharynx, in the pyriform sinuses and in the area of the ventricles of the larynx.
There are a number of features that distinguish the palatine tonsils from other lymphoid formations of the pharynx, which allows the palatine tonsils to occupy a special place in the physiology and pathology of the lymphadenoid pharyngeal ring. These signs are as follows.
In the palatine tonsils there are lacunae that turn into crypts, which branch in a tree-like manner up to 4-5 orders and spread throughout the entire thickness of the tonsil, while in the lingual and pharyngeal tonsils there are not crypts, but grooves or clefts without branches.
Lymphoepithelial symbiosis has its own characteristics: in all tonsils, except the palatine tonsils, it extends only to their surface. In the palatine tonsils, the lymphoid mass is in contact with the epithelium on a large surface of the crypt walls. The epithelium here is easily permeable to lymphocytes and antigen in the opposite direction, which stimulates the production of antibodies.
The palatine tonsils are surrounded by a capsule - a dense connective tissue membrane covering the tonsil on the lateral side. The lower pole and pharyngeal surface of the tonsil are free from the capsule. The pharyngeal and lingual tonsils do not have a capsule.
In the paratonsillar tissue of the upper pole of the palatine tonsils, Weber's mucous glands are sometimes located, which do not communicate with the crypts.
Lymphadenoid tissue undergoes reverse development over time. The pharyngeal tonsil undergoes involution starting from 14-15 years of age, the lingual tonsil reaches its maximum development by 20-30 years. Involution of the palatine tonsils also begins at 14-15 years of age and persists until old age.
The main function of the tonsils, like other lymphatic organs - lymph nodes, spleen, Peyer's patches of the intestine, etc., is the formation of lymphocytes - lymphopoiesis. Lymphopoiesis occurs in the centers of the follicles (germinal centers), then, upon maturation, lymphocytes are pushed to the periphery of the follicles, from where they enter the lymphatic pathways and the general lymph flow, as well as onto the surface of the tonsils. In addition to follicles, the formation of lymphocytes can also occur in the lymphoid tissue surrounding the follicles.
The study of the immunological role of the palatine tonsils has proven their participation in the formation of immunity (antibody formation), especially at a young age. This is facilitated by the fact that the location of the palatine tonsils on the path of the main entrance gate for various infectious pathogens and toxic products ensures close contact of the mucous membrane of the tonsils with the bacterial agent, and this, in turn, underlies the formation of immunity. The very structure of the crypts - their narrowness and tortuosity, the large total surface of their walls - contributes to long-term contact of antigens and lymphoreticular tissue of the tonsil.
It should be noted that, being an immune (antibody-forming) organ, the palatine tonsils under physiological conditions do not lead to significant permanent immunization of the body. The palatine tonsils make up only a small part of the lymphoepithelial apparatus located in other organs. The ability of the palatine tonsils to form antibodies is most pronounced in the period before puberty. However, in adults, tonsil tissue can retain this function.
The palatine tonsils perform an elimination function, participating in the removal of excess lymphocytes. The large area of contact between lymphadenoid tissue and the epithelium in the crypts plays an important role in the migration of lymphocytes across the surface of the mucous membrane of the tonsils, maintaining a constant level of lymphocytes in the blood.
Many researchers recognize the enzymatic function of the tonsils of the pharyngeal ring, in particular the palatine tonsils. Biochemical analyzes made it possible to detect various enzymes in the tissue of the tonsils, as well as in migrating lymphocytes - amylase, lipase, phosphatase, etc., the content of which increases after eating. This fact confirms the participation of the palatine tonsils in oral digestion.
The lymphadenoid pharyngeal ring has a close connection with the endocrine glands - the thymus, thyroid gland, pancreas, and adrenal cortex. Although the palatine tonsils do not have endocrine functions, there is a close relationship in the pituitary gland - adrenal cortex - lymphatic tissue system, especially before puberty.